Managing Symptoms & Side Effects
Treatments for cancer often cause side effects that impact your physical and mental health. Cancer-related fatigue, brain fog, trouble talking or swallowing and issues with sexuality and fertility might be some of these side effects. Your healthcare team at CancerCare Manitoba will discuss your symptoms and side effects with you, but you must tell them how you’re feeling. Nothing is too small to mention.
We also encourage you and your loved ones to watch the Living Well with Cancer-related Fatigue video series in the fatigue section below, which was a joint production of CancerCare Manitoba, Alberta Health Services and the Saskatchewan Cancer Agency. The series includes patients who share openly about their experiences with fatigue, as well as practical tips from healthcare professionals. It also covers other related topics such as stress, exercise, and nutrition.
Patient and Family Support Services offer programs, support groups, and resources related to a variety of symptoms and side effects. Please contact them for additional information at 204-787-2109 or toll-free at 1-866-561-1026.
Please look through the list below to see if one may help you:
(Note: This information does not replace the advice of your healthcare professional)

Brain Fog
Cancer patients have been reporting cancer-related cognitive changes for many years, with recent neuroimaging studies finding structural and functional changes in the brains of cancer patients.
Initially, patients coined the terms chemo brain and chemo fog to describe the cognitive changes they noticed after receiving chemotherapy. Over time, it became evident that cancer patients who had never received chemotherapy were also reporting cognitive changes, leading to the use of the terms cancer-treatment-associated cognitive change or cancer-related brain fog. Patients report problems with short-term memory, concentration, attention, word retrieval, and multi-tasking, which affect their quality of life.
Current studies don’t provide definitive answers about the cause of brain fog, but scientists believe it may be both host-related and disease-related.
While these cognitive changes do improve over time for most individuals, for a small subset of cancer patients the impairment may be sustained and impact their ability to function at work and home. Suggestions for treatment focus on health promotion, cognitive training, compensatory strategies, and restorative activities.
Patient and Family Support Services at CancerCare Manitoba offers patients an evidence-based program called Coping with Brain Fog. The popular and well-received program includes information and strategies to manage cancer-related cognitive changes.
For more information on upcoming sessions, which are also available through Manitoba Telehealth, please call Patient and Family Support Services at 204-787-2109 or toll-free at 1-866-561-1026.
Bleeding
What is the symptom?
Bleeding is when you lose some blood. Blood is a bodily fluid.
People can lose blood by:
- An injury or accident
- From some cancers
- Some cancer treatments can thin the blood and may make you bleed easier. Bruising is a form of bleeding under the skin.
Tips - What should I watch out for?
- Blood from the nose, mouth, vagina, or rectum
- Coughing up blood from the lungs
- Bruising on the skin
Constipation (unable to move your bowels)
What is the symptom?
Constipation is when you cannot have a bowel movement easily.
Tips - What should I watch out for?
- The stool (bowel movement) is hard and you may have to push to get it out.
- Abdominal (stomach) pain or cramps, or rectal pain (pain with having a bowel movement).
- There is a feeling that your bowel is not empty.
- Not having a bowel movement within three days.
- Vomiting (throwing up).
Diarrhea (runny or watery stool)
What is the symptom?
Diarrhea is liquid or watery stools or having very frequent bowel movements.
Tips - What should I watch out for?
- Loose or watery stools.
- Having more bowel movements in a day than you normally do.
Constipation & Diarrhea Information Translations
| Available Language | PDF Format | Audio Version | ||
|---|---|---|---|---|
| Constipation | Diarrhea | Constipation | Diarrhea | |
| English | View | View | Listen | Listen |
| French | View | View | Listen | Listen |
| Chinese | View | View | Listen | Listen |
| Cree | View | View | Listen | Listen |
| Filipino | View | View | Listen | Listen |
| Hindi | View | View | Listen | Listen |
| Inuktitut | View | View | Listen | Listen |
| Ojibwe | View | View | Listen | Listen |
| Oji-Cree | View | View | Listen | Listen |
| Portuguese | View | View | Listen | Listen |
| Punjabi | View | View | Listen | Listen |
| Spanish | View | View | Listen | Listen |
| Vietnamese | View | View | Listen | Listen |
Emotional Impact of Cancer
| Available Language | PDF Format | Audio Version |
|---|---|---|
| English | View | Listen |
| French | View | Listen |
| Chinese | View | Listen |
| Cree | View | Listen |
| Filipino | View | Listen |
| Hindi | View | Listen |
| Inuktitut | View | Listen |
| Ojibwe | View | Listen |
| Oji-Cree | View | Listen |
| Portuguese | View | Listen |
| Punjabi | View | Listen |
| Spanish | View | Listen |
| Vietnamese | View | Listen |
Living Well with Cancer-related Fatigue
For many patients, cancer-related fatigue is very different from the tiredness they experienced prior to their diagnosis. Sometimes it’s described as suffering because it’s more intense, severe and unrelenting than 'normal' fatigue.
We know that 70 to 90-plus percent of patients experience cancer-related fatigue and it has an impact on their physical, emotional, cognitive, social and spiritual well-being. “Many patients will say that it’s one of the most, if not the most, distressing symptom that they will experience,” says Dr. Joel Gingerich, a medical oncologist at CancerCare Manitoba.
Data from the COMPASS questionnaire filled out by patients at their CancerCare Manitoba appointments has helped us to better understand the effects of cancer-related fatigue.
We encourage you and your loved ones to watch the Living Well with Cancer-related Fatigue video series below, which was a joint production of CancerCare Manitoba, Alberta Health Services and the Saskatchewan Cancer Agency. The series includes patients’ candid experiences with fatigue, as well as practical tips from healthcare professionals.
CCMB also holds regular information sessions on coping with fatigue. To get information on the next session, or for other resources, please contact Patient and Family Support Services at 204-787-2109 or toll-free at 1-866-561-1026.
Living Well with Cancer-related Fatigue Video Series
Introduction
Module 1 - Find Support
Module 2 - Pace Yourself
Module 3 - Managing Your Stress
Module 4 - Exercise & Be Active
Module 5 - Nutrition & Eating Well
Conclusion
Fatigue Information Translations
| Available Language | PDF Format | Audio Version |
|---|---|---|
| English | View | Listen |
| French | View | Listen |
| Chinese | View | Listen |
| Cree | View | Listen |
| Filipino | View | Listen |
| Hindi | View | Listen |
| Inuktitut | View | Listen |
| Ojibwe | View | Listen |
| Oji-Cree | View | Listen |
| Portuguese | View | Listen |
| Punjabi | View | Listen |
| Spanish | View | Listen |
| Vietnamese | View | Listen |
Fertility
Many treatments for cancer can have an impact on your ability to have children in the future. Being able to have children after cancer depends on several factors. These include the type of cancer, the treatments given, how old you were when you were treated and how long it has been since you finished treatment for your cancer.
Male and female patients need to discuss their plans for having children with their oncologist or other healthcare providers as soon as possible. This also includes parents whose children are undergoing cancer treatments.
There are services available to preserve fertility, but you have to act quickly and before treatment starts.
Heartland Fertility Clinic in Winnipeg provides a variety of fertility services such as sperm banking, egg freezing and embryo preservation. Call 204-779-8888 or visit the clinic’s website at heartlandfertility.mb.ca for more information.
Fever
What is the symptom?
A fever is when your body temperature is higher than normal.
- A normal body temperature ranges from 35.6 to 38.2 degrees Celsius or 96.0 to 100.4 degrees Fahrenheit.
- It is important to monitor your body temperature.
Tips - What should I watch out for?
- Body chills (feeling like you cannot get warm), a cough, a sore throat or mouth, or burning feeling when you empty your bladder.
- Fever is a serious symptom that may mean you have an infection.
- If your temperature goes higher than 38 degrees Celsius or 100.4 Degrees Fahrenheit you need to seek medical attention.
Hair Loss (alopecia)
Hair loss can occur due to chemotherapy or radiation therapy treatments. Other hormonal or biological therapies can also cause the hair to become dry or thin. It's important to note that even though it is a common side effect, not all drugs cause hair loss. Hair loss in most cases is temporary and the amount of hair loss along with the time taken for regrowth depends on the length of treatment, the type of drug along with the dose and other personal factors.
CancerCare Manitoba’s Guardian Angel Caring Room is a place where you can receive help from compassionate, knowledgeable staff and volunteers. Our Caring Room offers a wig service, head coverings and laryngectomy stoma covers at no cost. They also offer a Look Good Feel Better Program that provides hands-on workshops for skincare, makeup, and head-covering techniques. Take a look.
Nausea
What is the symptom?
Nausea is feeling like you’re going to throw up.
Tips - What should I watch out for?
- Feeling like you’re going to throw up or be sick to your stomach.
- Feeling like you cannot eat or drink.
Vomiting
What is the symptom?
Vomiting is throwing up any food or liquids in your stomach.
Tips - What should I watch out for?
- You cannot keep any food or drinks in your stomach.
- Throwing up occurs even if you are not eating and drinking.
Nausea & Vomiting Information Translations
| Available Language | PDF Format | Audio Version |
|---|---|---|
| English | View | Listen |
| French | View | Listen |
| Chinese | View | Listen |
| Cree | View | Listen |
| Filipino | View | Listen |
| Hindi | View | Listen |
| Inuktitut | View | Listen |
| Ojibwe | View | Listen |
| Oji-Cree | View | Listen |
| Portuguese | View | Listen |
| Punjabi | View | Listen |
| Spanish | View | Listen |
| Vietnamese | View | Listen |
This information does not replace the advice of your healthcare professional.
Neuropathy
What is the symptom?
The body has many nerves in it. Nerves help us to move and feel things that we can see, hear, taste, smell, and touch.
Neuropathy (nerve pain) is an injury to the nerves in a part of the body.
Neuropathy can be caused by:
- Surgery.
- Health conditions. For example, cancer, and diabetes.
- Cancer treatments. For example, chemotherapy, and radiation.
Tips - What should I watch out for?
- A burning feeling or pain.
- Tingling or pins and needles feeling.
- Numbness or loss of feeling.
- An odd feeling in the area.
- Unsteady when you walk.
- Cannot button your shirt.
- Cannot pick up small objects.
- You may not be able to feel if something is too hot or cold and you can burn or freeze your skin.
Neutropenia
Neutropenia is defined as low numbers of germ-fighting neutrophils in the blood. Neutrophils are a type of white blood cell.
Neutrophils and other white blood cells help your body fight infection and repair damaged tissue. When the number of neutrophils in the blood becomes low, your body might find it harder to fight off infections.
If you have had chemotherapy in the past six weeks and have a fever, chills, cough or sore throat go promptly to your nearest emergency department or the Urgent Cancer Care Clinic or contact your health care team for directions.
The Importance of Good Nutrition
People with cancer often experience difficulty with eating, which can compromise their nutritional status. Malnutrition isn’t uncommon and can result from the side effects of cancer treatments, the effects of the tumour itself and even the emotional or social effects of being diagnosed with cancer. It’s important to maintain good nutrition before, during and after treatment to improve strength, well-being, and quality of life.
You may benefit from meeting with a CancerCare Manitoba registered dietitian specializing in oncology if you’re experiencing any of the following food-related discomfort or challenges:
- unwanted weight loss or weight gain;
- difficulty with food or fluid intake because of treatment side effects such as taste changes, dry mouth, nausea, diarrhea, constipation, or poor appetite;
- difficulty chewing or swallowing.
A dietitian can also help if you:
- would like to try commercial nutritional supplements or other specialized nutritional products to help improve your nutritional intake;
- have questions about unconventional nutritional products or therapies;
- have other medical conditions requiring a special diet such as diabetes, high cholesterol, high blood pressure, allergies, etc.;
- have general questions about healthy eating or a healthy diet after cancer treatment.
Nutrition education from a registered dietitian specializing in oncology is available for patients through CancerCare Manitoba in Winnipeg at the McDermot Site and the St. Boniface Hospital Site, as well as the Western Manitoba Cancer Centre in Brandon.
Please call:
- McDermot Site 204-787-2109 or 1-866-561-1026
- St. Boniface Site 204-787-1091 or 1-866-561-1026
- Brandon 204-578-2234
Patients can be referred by any member of their healthcare team or can arrange for an appointment themselves. Please call Nutrition Services at 787-2109 or toll-free at 1-866-561-1026.
Nutrition Information Translations
| Available Language | PDF Format | Audio Version |
|---|---|---|
| English | View | Listen |
| French | View | Listen |
| Chinese | View | Listen |
| Cree | View | Listen |
| Filipino | View | Listen |
| Hindi | View | Listen |
| Inuktitut | View | Listen |
| Ojibwe | View | Listen |
| Oji-Cree | View | Listen |
| Portuguese | View | Listen |
| Punjabi | View | Listen |
| Spanish | View | Listen |
| Vietnamese | View | Listen |
Pain
What is the symptom?
Pain is the feeling caused by something that hurts the body, for example, a fall or accident. Other words you may use to describe pain are ache or discomfort.
Some people may have pain from their cancer or cancer treatments.
Pain severity may range from mild to severe.
Pain may happen when you are doing things or when you are resting.
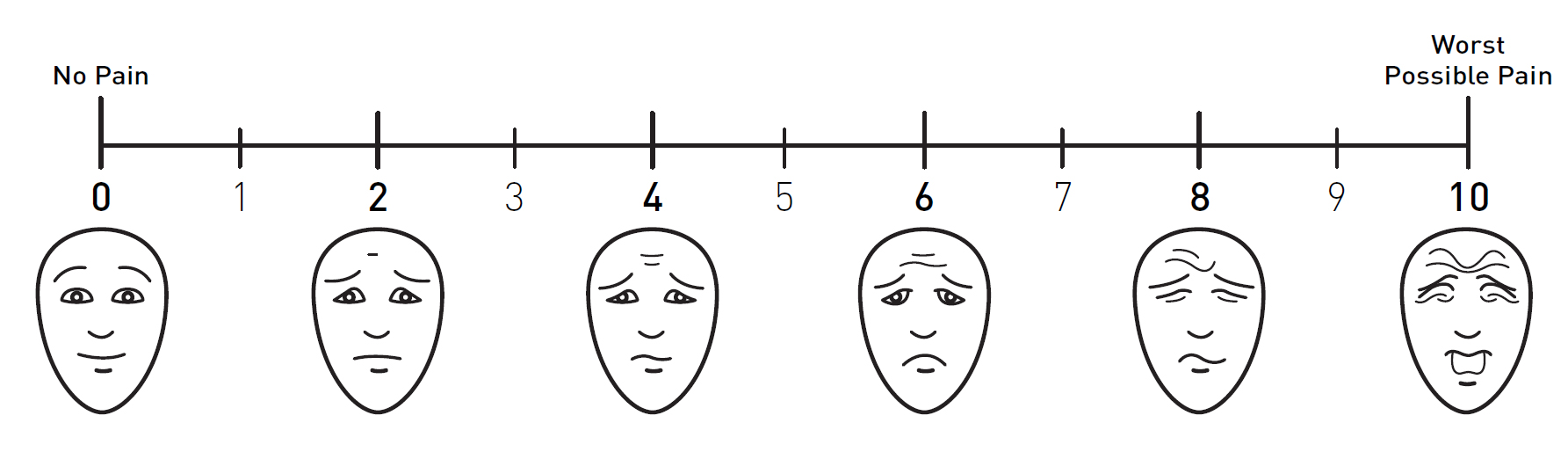
Check the Pain Scale below to help you tell us how much pain you feel.
Tips - What should I watch out for?
- Having pain somewhere in your body.
- Questions your health care team might ask about your pain:
- What does your pain feel like (dull, ache, sharp, stabbing, tingling)?
- What makes the pain get worse?
- What do you do to make it feel better?
- You can use pain medication to treat the pain.
- If pain medication does not help, call your nurse or doctor.
- Pain can make you feel:
- sick to your stomach,
- shaky,
- afraid or worried.
Pain & Symptom Clinics
Patients can experience many different problems or symptoms from their cancer that may need treatment. CancerCare Manitoba has two pain and symptom clinics you can attend and be cared for by health professionals familiar with your specific concerns.
These clinics, which work with the primary cancer team, are held at both the McDermot and St. Boniface sites in Winnipeg and can also be accessed through Manitoba Telehealth. Family members are considered integral to the assessment process and are encouraged to attend the clinic appointment with patients.
Here are some of the common symptoms that are assessed and treated at the clinics:
- pain
- nausea and vomiting
- shortness of breath
- constipation or diarrhea
- fatigue and weight loss
- depression, delirium, emotional suffering
Referrals can be made by family physicians, specialists, and nurses using the standard CancerCare Manitoba referral form. Download standard CCMB referral form.
For appointments, call 204-787-2176 or fax 204-786-0621.
Pain & Symptom Resources - Criteria for referral to the Pain and Symptom clinics.
Phone Consultation
A pain and symptom physician is available via telephone to aid in pain and symptom management during normal business hours from Monday through Friday.
The main purpose of this service is to give "over-the-phone" consultation promptly to members of the healthcare teams caring for cancer patients with significant symptom issues related to their cancer or cancer treatment.
To access the pain and symptom physician on call during business hours, call 204-237-2033.
Pain Handout and Diary
Physicians and patients may find it valuable to use a pain chart and pain diary so they can keep track of medication and its effect(s).
- Download a pain handout here.
- Download additional pain diaries here.
Radiation Skin Changes
What is the symptom?
Radiation treatments can cause side effects. This will depend on where the radiation is given and how much radiation you get.
Tips - What should I watch out for?
- Redness, itching or burning of the skin.
- The skin may be dry.
- Be wet (skin may open and leak).
- Peel.
- Blister (fluid-filled bubble of skin).
- Pain in the radiation area.
The Benefits of Exercise
Whether you're living with or are cancer-free, physical activity can:
- Help you feel better
- Reduce your risk of some cancers from coming back
- Reduce your risk of getting other cancers
Any amount of physical activity is good for you. Physical activity can include everything from walking or housework, to exercise programs at a gym or team sports. Your cancer type, treatment or any other conditions you have may affect the sort of activity that’s best for you. You can choose what types of activities to do and for how long. Consider what you like and your fitness level.
Being active during and after treatment can:
- Reduce tiredness (fatigue)
- Reduce depression
- Reduce stress and anxiety
- improve your quality of life
- Help you sleep better at night
- Help build muscle strength
- Help strengthen your bones
- Help reduce your risk of getting a blood clot
- Help relieve pain
- Improve range of motion
During treatment, you are the best judge of how much activity you can manage. It can be as simple as trying to reduce the amount of time you spend resting or starting with daily walks. After treatment, slowly increase your physical activity every week. Speak to your doctor or nurse about what is safe for you.
Follow the Canadian Physical Activity Guidelines by visiting the website: www.csep.ca
As you become active, here are some tips to stay safe while exercising:
- Don't exercise if you don't feel well or have any symptoms that worry you
- Use footwear that fits well and is made for the activity you are doing
- Drink plenty of water
- Avoid uneven surfaces and anything that might make you trip or fall
- Stop if you feel dizzy, have chest pain, a racing heart, breathing problems or any other sudden symptoms and contact your doctor.
You may also benefit from watching the Living Well with Cancer-related Fatigue video series, which includes a segment on exercise. The series is found in the fatigue section under Side Effects.
3 Minute Movement Videos
Cardio Workout
Lower Body Workout 1
Lower Body Workout 2
Upper Body Workout
Yoga Workout
Sexuality
Living with cancer can impact sexual functioning in various ways due to the disease itself, treatments, self-perception, and emotions. People with cancer often have questions about sexuality, which can evolve from diagnosis through treatment and recovery, and many seek support to maintain intimacy with their partners.
CancerCare Manitoba provides sexuality information and counselling services through Psychosocial Oncology (Counselling). Their team includes social workers, psychologists, psychiatrists, and other healthcare professionals. In Winnipeg, you can find them at the McDermot and St. Boniface sites. To schedule an appointment, call 204-787-2109 or toll-free at 1-866-561-1026. If you live outside Winnipeg, regional hubs offer support closer to your home. Visit the Psychosocial Oncology - Counselling page for more information.
Mouth Sores (Mucositis)
What is the symptom?
Mucositis is having a sore mouth or throat (Inflammation).
Tips - What should I watch out for?
- White spots in the mouth or on your tongue.
- Red sores in your mouth, on the tongue or the lips.
- Pain or burning in the mouth.
- Pain with swallowing food or liquids.
- Unable to wear your dentures.
Sore Mouth/Throat Information Translations
| Available Language | PDF Format | Audio Version |
|---|---|---|
| English | View | Listen |
| French | View | Listen |
| Chinese | View | Listen |
| Cree | View | Listen |
| Filipino | View | Listen |
| Hindi | View | Listen |
| Inuktitut | View | Listen |
| Ojibwe | View | Listen |
| Oji-Cree | View | Listen |
| Portuguese | View | Listen |
| Punjabi | View | Listen |
| Spanish | View | Listen |
| Vietnamese | View | Listen |
Trouble Talking or Swallowing
Some side effects of cancer treatments may be difficulties talking or swallowing. Speech-language pathologists at CancerCare Manitoba can provide assessment, treatment, and education for disorders of communication and swallowing. Their services are available at the McDermot and St. Boniface Sites in Winnipeg or two-way video conferencing through Telehealth.
Some typical communication problems experienced by cancer patients include:
- the voice is too quiet or becomes fatigued when talking too much;
- difficulty being heard and understood by others;
- having to repeat yourself often;
- difficulty concentrating on speech and putting sentences together;
- trouble remembering information.
A speech-language pathologist can help you find strategies to have clearer, more audible speech and voice, and to make understanding and speaking easier. You can also receive techniques for improving memory.
Cancer patients may also have difficulties swallowing. Signs and symptoms can include:
- * coughing or choking during or after eating solid food and/or drinking liquids;
- * weight loss;
- sense of food getting stuck;
- nasal regurgitation (food or liquids coming out of the nose);
- dehydration;
- weak cough;
- a lot of saliva or secretions;
- difficulty chewing;
- complaints or signs of discomfort during a meal.
A speech-language pathologist can help you understand your eating and swallowing difficulties. They can provide strategies to make swallowing safer and easier and help you avoid complications of swallowing difficulties such as weight loss, aspiration and lung infections. They can also assist you to improve swallowing skills and oral intake after cancer treatment, improve oral intake after tube feeding and reduce anxiety around swallowing concerns.
Speech-language therapists work closely with physicians, nurses, dietitians, and other healthcare professionals, who can make a referral for you.
For more information, please call Speech and Language Services at 204-787-2109 or toll-free at 1-866-561-1026 from Monday to Friday between 8:30 a.m. and 4:30 p.m.

