Medications to help quit
EN | FR
Nicotine replacement therapy (NRT)
When you quit smoking the level of nicotine in your body decreases causing you to feel withdrawal symptoms. Nicotine replacement therapy:
- is considered safe.
- is a way of getting nicotine without also taking in harmful chemicals.
- lessens withdrawal symptoms by slowly reducing the body’s need for nicotine.
- comes in different forms.
- can be used on their own or in combination with other nicotine replacement therapies.
IMPORTANT: Smoking cessation aids may interact with other medicines that you are taking. Tell the person who gave you the nicotine replacement therapy or prescription about all prescriptions, over-the-counter medicines, vitamins and herbal remedies that you take.
Nicotine patch
The nicotine patch sticks on your skin – usually your arm, back or chest. The nicotine patch slowly releases nicotine into your bloodstream. It is considered very useful for people with early morning cravings for cigarettes or tobacco. If you choose to use the nicotine patch, you can start using it on your quit day or as you start to reduce your number of cigarettes.
How to use:
- Apply to clean dry area of skin.
- Remove the old patch before putting on a new one.
- Choose a different area on your body to place the patch every day.
- Do not use lotion or moisturizing soap on the area where you apply your patch.
- Only touch the corners of the patch when applying.
- Press down on the patch after applying to ensure that all corners stick to your skin.
- Throw away the old patch by folding it over on itself and putting it in the trash can out of reach from children and animals.
Possible side effects: May cause skin irritation, itchiness, headaches, and insomnia. Any irritation or itchiness should resolve within a few minutes after applying the patch.
.
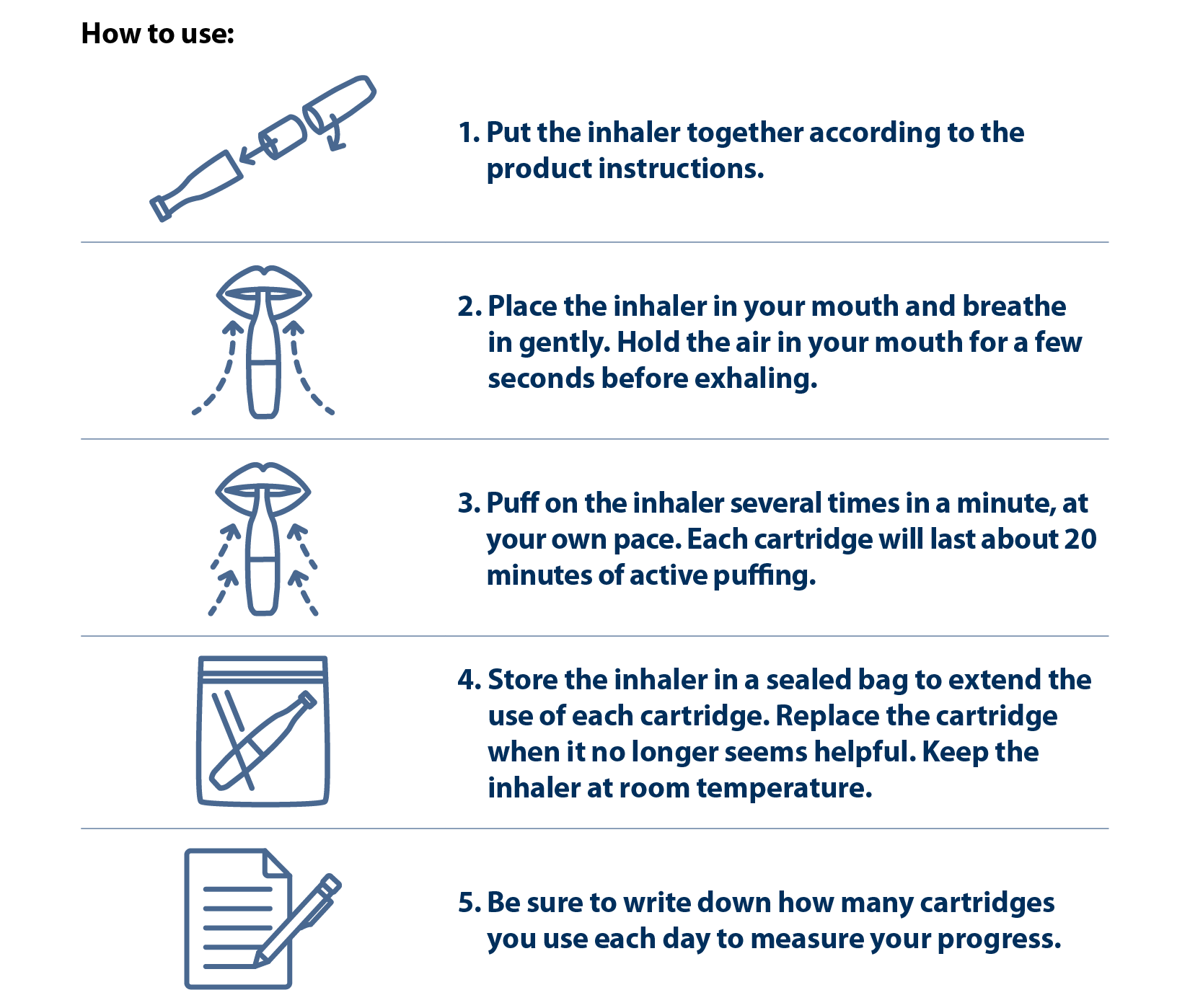
Nicotine inhaler
The nicotine inhaler is a plastic tube with a nicotine cartridge inside. If you choose to use the nicotine inhaler, you can start using it on your quit day or as you start to reduce your number of cigarettes.
Possible side effects: Throat or mouth irritation, headaches, upset stomach, vomiting, blurred vision, dizziness, and drooling.
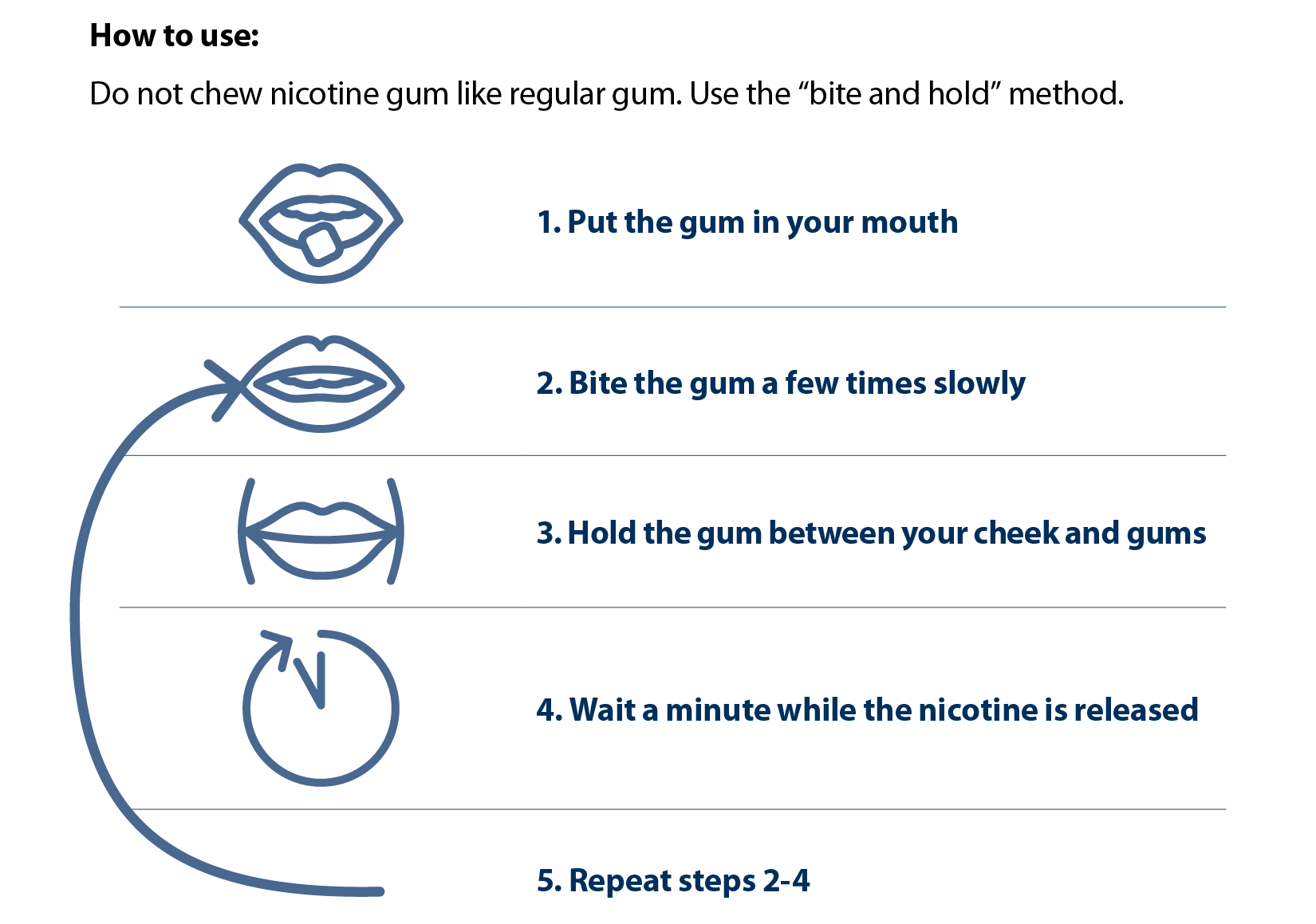
Nicotine gum
Chewing nicotine gum releases nicotine into your bloodstream. The gum is not recommended for people who have dentures, or people with throat, mouth, or jaw problems. The nicotine in the gum will typically be released over 30-60 minutes. After this, it should be thrown out. If you choose to use nicotine gum, you can use it on your quit day.
Possible side effects: Mouth or jaw soreness, hiccups, and upset stomach.
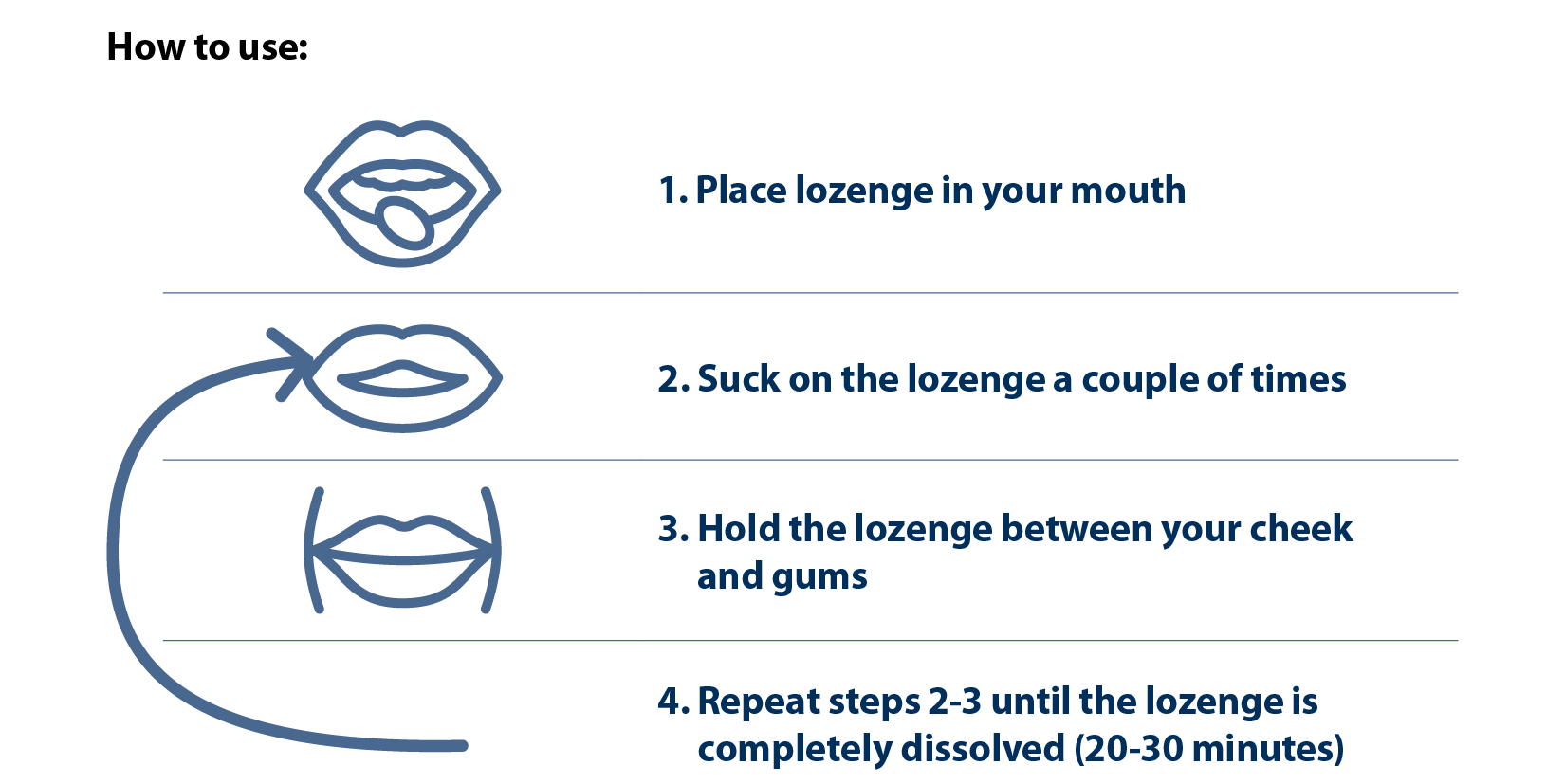
Nicotine lozenge
Nicotine is absorbed into your bloodstream when you suck on a nicotine lozenge. The lozenge should not be chewed or swallowed. If you choose to use the nicotine lozenge, you can use it on your quit day.
Possible side effects: Mouth soreness, hiccups, and upset stomach.
Can I have too much nicotine?
The answer is yes, but it is uncommon. Combining more than one type of NRT (e.g. patch and inhaler/gum/lozenge) would not be enough to cause a nicotine overdose.
People who smoke less than 10 cigarettes per day will usually use less NRT. You should try to completely stop the use of cigarettes while on NRT. The risk of side effects is higher if you continue to smoke your usual amount of cigarettes while on NRT.
If you are experiencing the following symptoms all at once, this could be because you have had too much nicotine.
- Abdominal pain
- Drooling
- Nausea
- Headaches
- Cold sweat
- Dizziness
If you experience side effects while using nicotine products, your healthcare provider can make changes to help you feel better and receive the most benefit.
Other medicines
There are medicines other than nicotine replacement therapies that can be used to help you quit smoking. These work by reducing the satisfying feeling provided by nicotine. This makes smoking less enjoyable while reducing your cravings and nicotine withdrawal symptoms. Two of the medications to help you stop smoking are varenicline and bupropion. These medications require a prescription from a healthcare provider. Varenicline and Buproprion would not be used at the same time.
Varenicline
Varenicline is a pill commonly known as Champix®. If you use varenicline, you must decide on a day that you will stop smoking. Once you pick a quit date, start taking varenicline one week before that date. This will give your body time for the medication to work effectively.
How to use:
- Follow instructions on the prescription
- Swallow pill with a meal and large glass of water to reduce the chance of having an upset stomach
Possible side effects: Upset stomach, trouble sleeping, abnormal or vivid dreams, headache, constipation, heart problems, depression, and suicidal thoughts.
Who should not use varenicline? Those with kidney problems and those who are pregnant or breastfeeding.
Bupropion
Bupropion is commonly known as Zyban® and is available in the form of a pill. If you decide that you would like to try bupropion, you must decide on a day that you will stop smoking. Once you pick a quit date, start taking bupropion one week before that day. This will give your body time for the medication to work effectively.
How to use:
- Follow instructions on the prescription.
- Swallow the pill whole. Do not crush or chew the pill.
Possible side effects: Upset stomach, trouble sleeping, dry mouth, drowsiness, dizziness, headache, anxiety, sweating, fast or irregular heartbeat, seizures.
Who should not use bupropion? Those who have seizures, bulimia, anorexia, or psychiatric problems, and those who are pregnant or breastfeeding.

