CervixCheck
EN | FR
Cervical Cancer
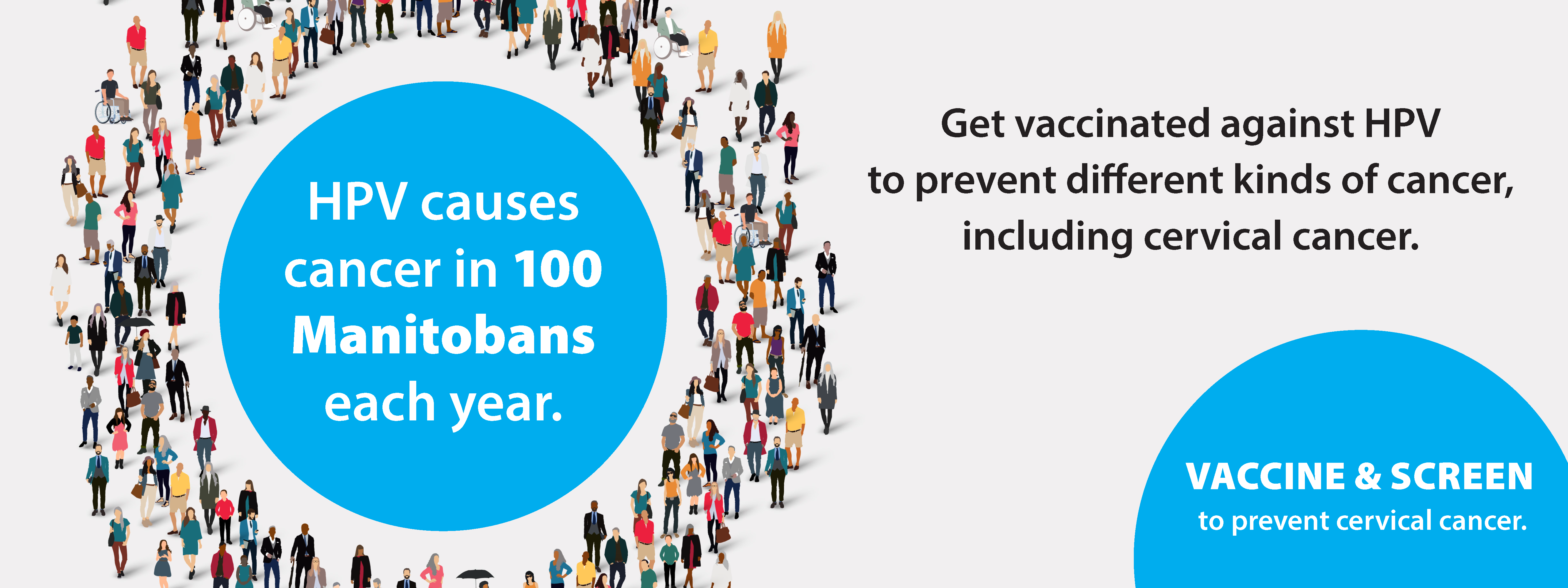
Cervical cancer is caused by human papillomavirus (HPV). Over 80% of Canadians will have at least one HPV infection in their lifetime.
Age 21-69?
Most women age 21 to 69 who have ever had sexual contact should have a Pap test every 3 years. Trans, non-binary, and gender diverse people with a cervix should have a Pap test every 3 years.
Get a CervixCheck!
Book an appointment with your regular healthcare provider, or find a Pap test clinic near you!
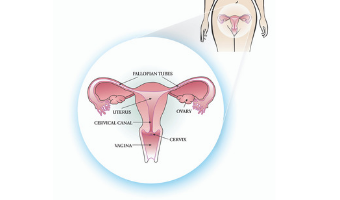
The cervix:
- is part of the female reproductive system.
- connects the vagina to the uterus.
- allows menstrual blood to pass during menstruation.
- allows sperm to pass into the uterus to fertilize and egg.
- stretches open during childbirth to allow a baby to pass through into the vagina.
Cancer is a serious illness in the body. Cervical cancer can occur when there is uncontrolled growth of cells on the cervix.
Cervical cancer is caused by high-risk human papillomavirus (hrHPV). HrHPV can cause abnormal cells to develop on the cervix. If the abnormal cells do not go away on their own, and/or if left untreated, they can become cancer.
Most people are at average risk of cervical cancer and should have a Pap test every 3 years.
Some people are at increased risk for cervical cancer and may need to be screened more frequently. Factors you cannot change that can increase your risk for cervical cancer include having a personal history of:
- human immunodeficiency virus.
- transplantation with immunosuppressive therapy for more than 3 years.
- exposure to diethylstilboestrol (DES) in utero.
- a previous high-grade cervical pathology (not Pap test) result.
To reduce your risk of cervical cancer:
Get checked for cancer
- Most women age 21-69 who have ever been sexually active should have a Pap test every three years to check for cervical cancer.
- Transgender and non-binary people may need to be screened for breast and cervical cancers.
Get vaccinated against HPV
- The HPV vaccine provides protection against certain types of low and high-risk types of HPV that can cause genital warts and cancer.
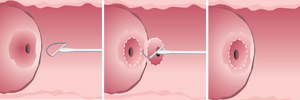
The Pap Test
A Pap test is a test that can find abnormal changes on the cervix before they turn into cancer. During a Pap test, cells are taken from your cervix, and sent to a lab for assessment. In most cases, the cells are normal. Sometimes abnormal changes caused by human papillomavirus (HPV) can become cancerous. Regular Pap tests with follow-up with abnormal changes can prevent most cancer of the cervix.
Step 1
You will be asked to undress from the waist down and lie on an exam table with your feet resting in the foot rests. Allow your knees to fall away from each other.
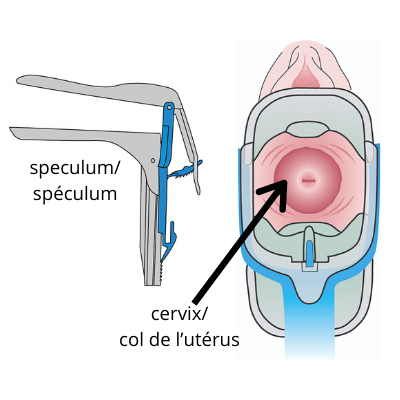
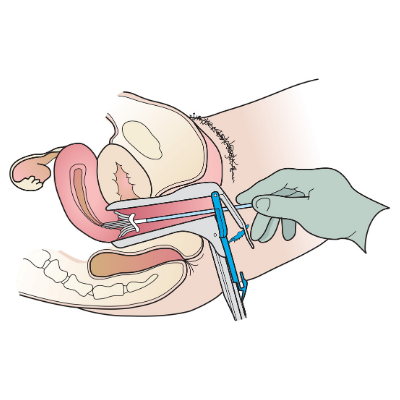
Step 2
A speculum is used to open the vagina and examine the cervix. Breathe deeply to help calm your muscles. This allows the speculum to be inserted more easily. You may feel some discomfort, but you should not feel pain. If you feel pain, be sure to let your doctor or nurse know.
Step 3
A small broom-like device is used to collect cells from the cervix.

Step 4
Cells are dropped into a vial and sent to a laboratory to be examined.
The speculum will be removed.
You can get dressed.
Potential Benefits
- Regular Pap tests with follow-up for abnormal changes can prevent up to 80% of cervical cancer
- Abnormal changes can be removed with procedures during colposcopy
- Detecting cancer at an early stage can result in simpler treatment, more treatment options, and less need for chemotherapy
Potential Harms
- Discomfort or bleeding from the Pap test or colposcopy
- Anxiety that may result from abnormal test results
- Over-diagnosis of abnormal cell changes that would go away on their own
- Problems with future pregnancies from some treatment during colposcopy
Results
Cervical cancer screening results are usually available 2-4 weeks after the test. You can get your result by:
- Contacting the doctor or nurse who did your test, or
- Requesting a copy of your result from CervixCheck.
Although most cervical cancer screening test results are normal, about one in 10 tests come back as abnormal. Most of the time, abnormal changes will disappear on their own without any treatment.
Your cervical cancer screening result will include a Pap test result and, depending on your age, may also include an HPV test result.
What does my Pap test result mean?
Normal: No abnormal cells were found. Nine out of ten times, Pap test results are normal.
Abnormal: Abnormal cells were found. An abnormal result does not mean you have cervical cancer or will get cervical cancer. It means that when the cells were examined under a microscope, they did not look normal. More testing is needed to understand the abnormal cells and possibly treat the cell changes.
What does my HPV test result mean?
High-risk HPV negative – No high-risk strains of HPV were detected. Your risk of cervical cancer is very low.
High-risk HPV positive – One or more strains of high-risk HPV was detected. A positive hrHPV result does not mean you have cervical cancer or will get cervical cancer. It means that you need to be seen by a colposcopist for further investigation.
Follow-Up Testing
If you have an abnormal result, you will need follow-up testing. Follow-up testing will be scheduled by your healthcare provider. It is important that you attend all follow-up appointments if you after an abnormal cervical cancer screening result.
Follow-up tests may include:
- Repeating your Pap test in 3-6 months, or
- Being referred to a colposcopy clinic.
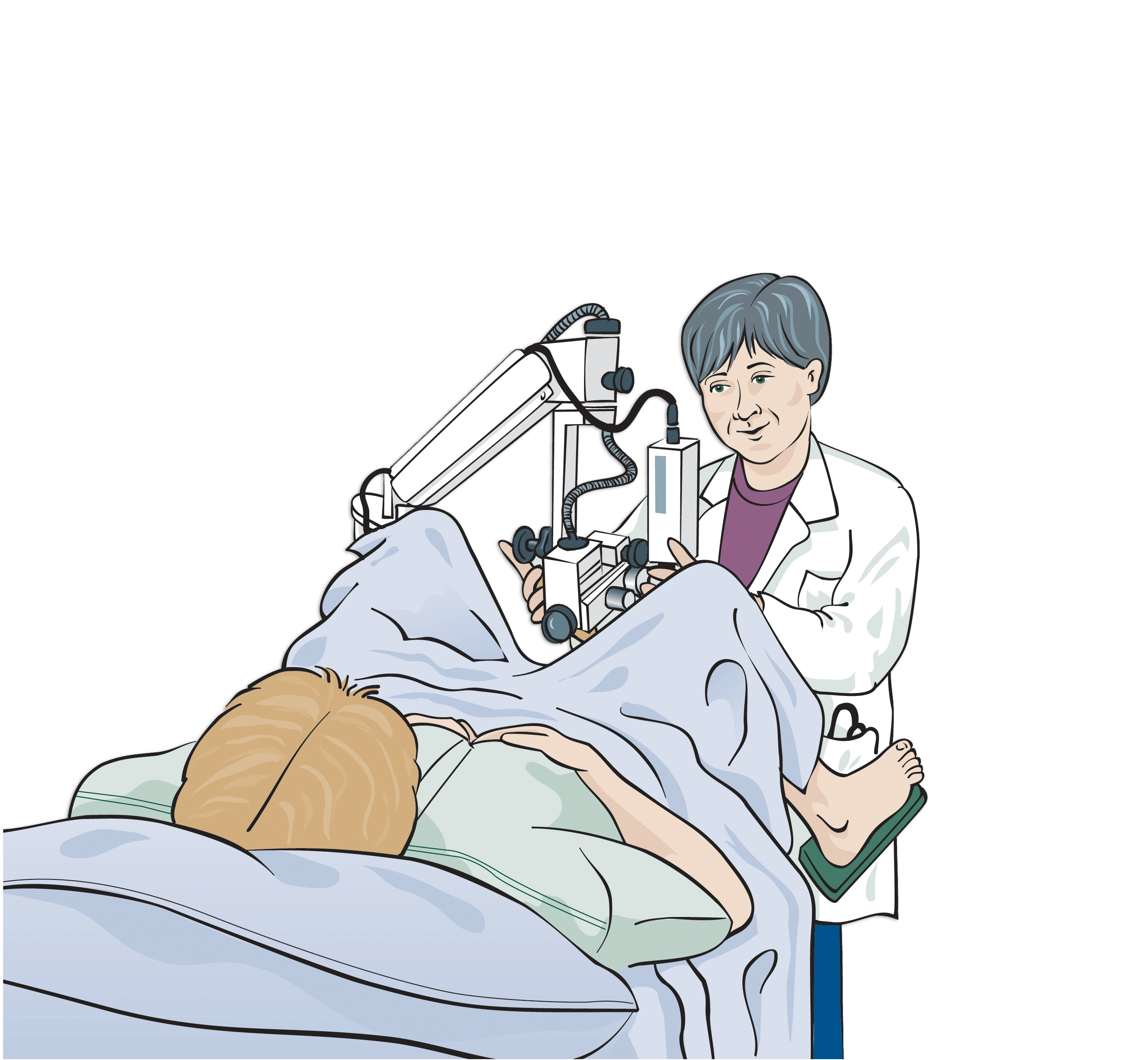
Colposcopy
In colposcopy, a colposcopist, a specially trained gynecologist, examines the cervix and vagina using a low-powered magnifier called a colposcope.
Preparing for a colposcopy appointment
- The colposcopy clinic will notify you of your appointment date, time, and address.
- Determine how you will get to your appointment and where you will park for your appointment.
- You can have colposcopy if you are pregnant, have an IUD, or have your period.
- If you need to change or cancel your colposcopy appointment, call the colposcopy clinic.
Colposcopy is like a Pap test.
- You lie down on the exam table and put your feet in supports.
- A speculum is put in your vagina so the cervix can be seen.
- The doctor looks at your cervix using a colposcope. The colposcope stays outside of the body.
- A tissue sample (biopsy) may be taken to see if treatment is needed.
- Tell the nurse or doctor if you are allergic to iodine or shellfish.
The doctor will remove the tissue sample during the colposcopy. The sample is very small (1-2 millimeters in size). The sample is removed with an instrument like a pair of tweezers and is sent to the laboratory.
Will a biopsy hurt?
A biopsy usually takes only a second. Some people feel nothing when they have a biopsy. Other people feel pinching or cramps. The pain usually stops within a few minutes. Your doctor may suggest a pain reliever.
Does a biopsy have any after-effects?
You may have spotting (small amounts of blood) for a few days. If you have spotting, use pads, not tampons.
For at least two days after your biopsy:
- Do not douche
- Do not have sexual intercourse
- Do not use tampons
The colposcopist will tell you if you need treatment.
Types of treatment
LEEP (loop electrosurgical excision procedure
After numbing the area with local anesthetic, an electrical wire loop takes the abnormal cells out of the cervix. After a LEEP, you may see a dark discharge for up to a week.
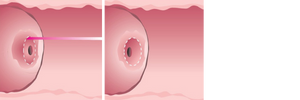
Laser Surgery
Laser surgery is a treatment that uses a laser beam (an intense narrow beam of energy) to remove abnormal cervical cells. A local anesthetic (freezing) is used. A watery discharge is a common side effect that may last up to two weeks.
After a colposcopy treatment
- You can usually return to work and most daily activities after your appointment.
- Do not do any strenuous exercise or heavy lifting for 2 days.
- For 3 weeks after laser surgery:
- Do not put anything in your vagina (e.g. no douching, sex, tampons).
- Do not have a bath in a tub.
- Do not use hot tubs or go swimming.
- Some vaginal bleeding or discharge is normal.
- If you are having more bleeding than expected after a colposcopy treatment (e.g. soaking one pad per hour for two or more hours), contact the colposcopy clinic or go to your nearest emergency room.
- Contact your doctor if:
- you have pain that is not relieved by Tylenol or Advil
- you have a fever (temperature of 38 degrees Celsius or 100 degrees Fahrenheit)
- you have foul smelling discharge.
- An HPV test may be done after the treatment to:
- see if you need another colposcopy appointment, or
- see if it is safe to stop colposcopy appointments (send you back to regular Pap screening).
- Your colposcopist will contact you with your result within 4 to 6 weeks of your appointment. If you have not been contacted within 6 weeks, you can call the colposcopy clinic.
If you have questions about your colposcopy appointment or result, call the colposcopy clinic.
For more information, see the following resources:
What you need to know about preventing cervical cancer (pdf)
Cervical cancer screening test result brochure - English/French*
HPV frequently asked questions - English
HPV frequently asked questions - French
Colposcopy - see videos below
To learn more about colposcopy, please review:
- What you need to know about preventing cervical cancer (PDF)
- Colposcopy videos (see below)
If it has been two to six weeks since your cervical cancer screening test, you can request your results in one of three ways:
1. Call CervixCheck toll-free at 1-855-952-4325.
2. Email your request to [email protected]
3. Complete an online request form on our website.
The registry is a confidential record of cervical cancer screening tests and follow-up test results for all Manitobans. The registry contains:
- your name, address and date of birth,
- your Personal Health Identification Number (PHIN) and your Manitoba Medical Number (MHSC),
- the date(s) of your test(s) and results,
- the name, address and number of the health care provider who did your test(s), and
- the name of the laboratory where each test was read.
The registry is accessed by:
- The health care provider who takes collects your cervical cancer screening sample,
- The laboratory that reads your cervical cancer screening sample, and
- CervixCheck staff involved in the registry.
Everyone who has access to your information is bound by the Personal Health Information Act (PHIA) and has signed a pledge of confidentiality.
Your personal health information is collected according to a regulation of the Public Health Act. For more information about your rights under the Personal Health Information Act, contact the Privacy Officer for CancerCare Manitoba at (204) 787-2266 or the Manitoba Health Legislative Unit at (204) 788-6612.
The Registry:
- keeps a record of all cervical cancer screening tests and follow-up tests done for you after April 27, 2001,
- allows you to obtain your own test results,
- sends your health care provider a letter if you fail to get recommended follow-up testing when an abnormality has been found,
- sends you a letter if follow-up is outstanding for an abnormal cervical cancer screening test result or if you are overdue for cervical cancer screening,
- collects information to improve our understanding of cancer of the cervix, and
- helps us to improve cervical cancer screening test services across Manitoba.
Keeping records becomes important if you move or change health care providers, or if your health care provider moves or changes laboratories. When looking at test results, medical staff should take your past history into account.
Opting In/Out of Registry
To opt out, indicate this in this CervixCheck Registry form (pdf) and return it to CervixCheck. We encourage you to discuss your decision with your healthcare provider or with CervixCheck. To opt back into the registry, please call our office. Your test results will be available to the registry from the date that you reenter the program.
The HPV Vaccine
The HPV vaccines provide protection against certain types of HPV that can cause genital warts, cervical cancer, as well as cancers of the mouth, throat, anus, vulva, vagina and penis. If an HPV vaccine is received before sexual contact, it will be almost 100% effective in preventing infection (see table below). Studies show that females who have already been sexually active may also benefit from receiving the vaccine.
There are three HPV vaccines approved for use in Canada:
| HPV types covered | Protects against: | |
|---|---|---|
| Cervarix | 16, 18 | Over 70% of cervical cancers |
| Gardasil 9 | 6, 11, 16, 18, 31, 33, 45, 52, 58 |
90% of cervical cancers & 90% of genital warts |
Females who receive the HPV vaccine still need to have regular Pap tests because the HPV vaccines do not protect against all HPV types that can cause cervical cancer.
It’s important to know that:
- None of the HPV vaccines can be used to treat existing HPV infections.
- Regular cervical cancer screening is important because HPV vaccines do not protect us from all types of HPV that can cause cervical cancer.
- Learn more about the HPV vaccine.
Should You Get the HPV Vaccine? (Dr. Mike Evans)
If you have these symptoms...
Contact your health care provider if you experience any signs or symptoms of cervical cancer and they last for 3 or more months.
Abnormal bleeding:
- unusually long or heavy periods,
- bleeding between periods,
- pain and/or bleeding during or after intercourse
- bleeding or spotting after menopause
Abnormal pain:
- persistent pelvic pain that radiates down one or both legs
- pain during or after intercourse
Abnormal discharge:
- foul smelling discharge
Pap Test Clinics
To book a Pap test appointment:
- contact your regular health care provider, or
- enter your postal code in the search box below and click the search icon to find a Pap test clinic near you.
Call ahead to the site to ensure the clinic will meet your Pap test needs. If you would like to promote a Pap test clinic in your community, we invite you to use our Cervical Cancer Screening Test Clinic Posters.
For help, call CervixCheck at 1-855-95-CHECK.
Bring your Manitoba Health Card to all your CancerCare Manitoba Screening appointments. Keep the information on your Manitoba Health card current. This will enable us to send you letters to remind you to get screened for cancer. To learn more, visit the Manitoba Health Card website.
Contact
If you would like to promote any of our campaign videos, radio, and social media posts, email [email protected]

