BreastCheck
EN | FR
Breast Cancer
Breast cancer is one of the most commonly diagnosed cancers in Manitoba women. Screening mammograms can find breast cancer early, when there may be more treatment options and a better chance of a cure.
Age 50-74?
Most women age 50 to 74 should have a screening mammogram every 2 years. Trans, non-binary, and gender diverse people may also need regular mammograms.
Get a BreastCheck!
Is it time for a screening mammogram? Call BreastCheck at 1-855-952-4325 to make an appointment.
Breast Cancer
Breast or chest tissue is made up of fatty, connective, and glandular tissue..
Every year 900 Manitoban women are diagnosed with breast cancer and 200 will die from the disease.
Only 10% of women diagnosed with breast cancer have a family history of breast cancer.
Eight out of ten breast cancers occur in women age 50 or older.
BreastCheck is a program that checks Manitoba women ages 50 and over for early signs of breast cancer. Regular screening mammograms are the best way to find breast cancer early. When found early, there may be more treatment options and better chance of a cure.
Cancer screening targets a specific group of people (e.g. age, sex) to maximize the potential benefit and minimize the potential harm of a screening test.
Talk with your health care provider about your individual risk for breast cancer.
Most people are at average risk of breast cancer should have a screening mammogram every 2 years.
Some people are at increased risk for breast cancer and may need to be screened more frequently. When you come for your first BreastCheck screening mammogram, we will ask you a series of questions to determine how frequently you should be screened for breast cancer. Factors you cannot change that can increase your risk for breast cancer include:
- Strong family history of breast cancer or ovarian cancer.
- Having a BRCA1 and/or BRCA2 gene mutation.
- Personal history of:
- lobular carcinoma in-situ,
- atypical ductal hyperplasia,
- atypical lobular hyperplasia,
- ovarian cancer,
- breast cancer, or
- radiation therapy in childhood or young adulthood.
Women can be screened at BreastCheck if they are 50 years of age and over and:
- do not have breast symptoms such as unusual lumps or bloody nipple discharge,
- do not have a personal history of breast cancer, and
- do not currently have breast implants.
Women who are not eligible to be screened at BreastCheck should speak with their health care provider about the best breast health care for their individual needs. Women who have symptoms of breast cancer should be referred to a diagnostic mammogram clinic by a health care provider for further testing.
To reduce your risk of breast cancer:
Maintain a healthy weight
- Maintain a weight within the healthy range.
Eat healthy
- Eat plenty of fruits and vegetables, whole grains, beans and lentils.
- Limit fast foods, highly processed foods, sugar-sweetened drinks and red meat.
Move more
- Be physically active for at least two and a half hours per week.
- Avoid sitting for more than six hours a day.
Avoid alcohol
- It is best not to drink alcohol. The less alcohol you drink, the more you reduce your risk.
Live smoke free
- Do not start smoking, quit smoking, and avoid second-hand smoke.
- Keep tobacco sacred. Do not smoke commercial tobacco.*
.
Get checked for cancer
- Most women age 50-74 should have a screening mammogram every two years to check for breast cancer.
*Commercial tobacco smoke contains more than 7,000 chemicals, at least 250 of which are known to be harmful and over 70 can cause abnormal cell growth which can then become cancer. Traditional tobacco is unprocessed, natural tobacco gathered and used by some Indigenous peoples as a part of their cultures. Traditional tobacco is considered a sacred plant with immense healing and spiritual benefits in some Indigenous cultures, where it is used for rituals, ceremonies, and prayers. When commercial tobacco is used instead of traditional tobacco, it can be harmful.
A Screening Mammogram
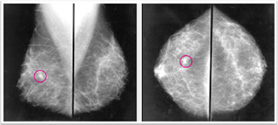
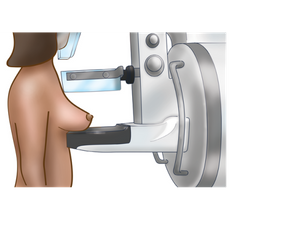
A mammogram is an x-ray of the breast tissue. An x-ray is a type of radiation that can pass through the body and is used to make an image of the tissue and bones. A mammogram image shows the detail of breast tissue from two different angles.
On the day of your mammogram appointment:

Do not wear deodorant.

Wear a two piece outfit.
What can I expect at my mammogram?
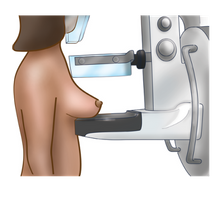
- A mammogram appointment takes between 10 and 20 minutes.
- A female technologist will ask you some health questions.
- You will need to remove your top and bra for the mammogram.
- A mammogram image shows the detail of your breast tissue from two different angles.
- During your mammogram:
- Each breast is positioned between two plastic plates on a mammogram machine.
- The plates are pressed together to flatten your breast. This is called compression. You may have discomfort, but know that it only lasts for a few seconds.
Breast compression:
- is not harmful to your breasts.
- is used to get a clear image of the breast tissue.
- reduces the amount of radiation needed for the mammogram.
- is tolerable for most clients.
What can I expect after my mammogram?
- Uou may experience redness or bruising; this usually disappears in a few days.
- Rarely, there may be some tearing of the thin skin under the breast.
- If you experience problems that do not go away after a few days, see your healthcare provider.
- If you have questions about your appointment or results, you can contact BreastCheck.
In the days after your mammogram, a radiologist will look at your mammogram images. Within two weeks of your mammogram, you and your healthcare provider will receive your results. Results will be either normal or abnormal. Information about breast density will also be included wiht your results.
Screening vs. Diagnostic Mammogram
The type of machine used and the process to get the first four images is the same for a screening or diagnostic mammogram. More images may need to be taken in a diagnostic mammogram to look at a specific area more closely, and different types of tools may be used to compress the tissue in different ways. BreastCheck offers screening mammograms for those age 50 to 74. Call 1-855-952-4325 to see if you are eligible to have a screening mammogram at BreastCheck.
Potential Benefits & Potential Harms of Breast Cancer Screening
For women of average risk, research shows that the potential benefits of breast cancer screening with mammography outweigh the potential harms. BreastCheck recommends most women age 50-74 have a screening mammogram every 2 years.
Potential Benefits
Research shows that regular screening mammograms reduce deaths from breast cancer in women age 50 to 74 by 20-30%.
This is due to early detection. Most breast cancers discovered through regular screening are found at an earlier stage when there may be more treatment options as well as more positive outcomes.
Potential Harms
Breast screening does not prevent breast cancer. A mammogram can only find breast cancer if it is already there. Some women may develop breast cancer before their first mammogram or between mammograms.
It is important to know how your breasts normally look and feel. Contact your healthcare provider if you notice any changes in your breasts between screening appointments, even if you had a normal screening mammogram.
- False Negatives - Mammograms do not find all breast cancers. 20 out of every 100 breast cancers cannot be seen on a mammogram, some cancers are very difficult to see on a mammogram, and/or the radiologist reading the mammogram may not see cancer (this happens occasionally no matter how experienced the doctor is). Breast density is a risk factor that may make it harder to see breast cancer on a mammogram. Effective June 2019, breast density will be included on your mammogram result letter, which is sent to you and your healthcare provider. Learn more about breast density categories (pdf).
To obtain the breast density category from:- your most recent BreastCheck mammogram, wait for your result letter.
- the BreastCheck mammogram prior to your most recent mammogram, complete the Personal Health Information Access Request form and send to BreastCheck at #5-25 Sherbrook Street, Winnipeg, MB, R3C2B1.
- your most recent BreastCheck mammogram, wait for your result letter.
- False Positives -About 5 out of every 100 women screened at BreastCheck will be sent for further tests. Only 1 of these 5 women will be diagnosed with breast cancer.
- Overdiagnosis -Mammograms are not guaranteed to save your life. Not all breast cancers found at screening can be cured. Some women will die of breast cancer even though it was found by a screening mammogram; some will die of something else before they would die of breast cancer. For these women, their quality and length of life may not be increased by finding the breast cancer. There is no way to know which women will fall into these groups and which women will be truly helped by screening.
- Distress - Breast cancer screening and follow-up testing can includes harms of discomfort, pain, and anxiety.
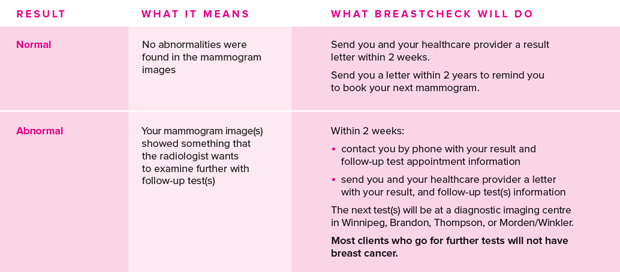
Results
In the days after your mammogram, a radiologist will look at your mammogram images. Within 2 weeks of your mammogram, both you and your healthcare provider will receive your results. Results will be either normal or abnormal.
No result letters will be mailed due to the Canada Post strike. Clients with abnormal screening test results will be contacted by phone.
Some women may be asked to return in 1 year. The most common reasons for this are:
- High or low increased risk based on family history of breast and/or ovarian cancer.
- The radiologist thinks it is best for the woman to come more often based on their clinical assessment.
- It is the woman's first mammogram and we do not have other mammograms to compare.
BreastCheck will send you a letter to remind you when it is time to book your next appointment. Call us if you do not receive a letter.
Even if you have a normal mammogram result, if you notice any changes to your breast tissue from how your breasts normally look and feel, you should contact your healthcare provider.
CLICK CHART ABOVE TO ENLARGE
Your mammogram report will also note your breast density. Breast density is how breast tissue appears on a mammogram image. Breast tissue is made up of two types of tissue: glandular and connective (dense) tissue and fatty (non-dense) tissue. A person’s breast tissue may be called dense if they have more glandular tissue than fatty tissue. BreastCheck categorizes breast density into one of four categories:
a) almost all fatty tissue
b) mainly fatty tissue with some scattered areas of dense tissue
c) a mixture of fatty and dense tissue
d) almost entirely dense tissue
To request your breast density information click here to complete a request for information. The request can be mailed or emailed to BreastCheck.
If you have dense breasts and are concerned about your risk of developing breast cancer, you should discuss your personal risk factors with your healthcare provider.
Follow-Up Testing
A mammogram image may show something that the radiologist wants to check with a follow-up test(s). It is normal to be a little scared, but it is important to know that most women who go for further follow-up testing do not have breast cancer.
1- Referral
You will be directly referred to one or more of the following places for additional test(s):
- WRHA Breast Health Centre
- Manitoba X-Ray Clinic
- Radiology Consultants of Winnipeg
- Brandon Regional Health Centre
- Thompson General Hospital
- Boundary Trails Health Centre
- Health Sciences Centre
2- Follow-Up Test(s)
You will be provided with more information about your specific test(s), how to prepare and how you will receive the results by the place to which you are referred.
Most clients who need further testing have one or both of these tests:
A) Diagnostic Mammogram
A diagnostic mammogram experience is very similar to a screening mammogram. The diagnostic mammogram takes a closer look at a specific area of breast tissue by:
- taking x-ray images from different angles than the standard angles in screening mammography,
- applying extra pressure to thin out a small specific area of breast tissue so it can be seen more clearly, or magnifying a specific area of breast tissue.
B) Ultrasound
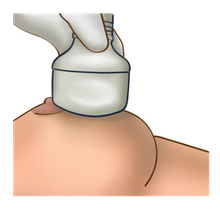
A breast ultrasound uses sound waves to create an image of the breast. During an ultrasound, a small amount of gel will be placed on your breast. A small probe (wand) will glide over the skin on your breast(s). The image can show if the lump is solid or filled with fluid.
A small number of patients will need a biopsy in addition to a diagnostic mammogram and/or ultrasound. A biopsy removes a small piece of breast tissue for testing. There are two main types of biopsy:
A) Ultrasound Core Biopsy
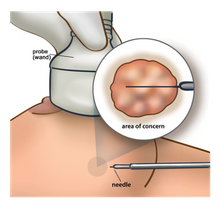
An ultrasound core biopsy uses a needle to remove tissue for testing when a lump can be felt, or seen on an ultrasound.
- A probe (wand) will be pressed against your breast to create an image and find the area of concern. You will feel some pressure on your breast.
- A small amount of local anesthetic (freezing) is injected into your breast with a needle. You will feel a sting.
- A small cut will be made in the breast area where the tissue will be removed.
- You may hear a click as the tissue samples are collected (biopsy).
- A bandage is placed over the skin opening.
B) Stereotactic Core Biopsy
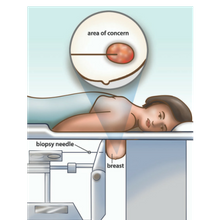
A stereotactic core biopsy uses a needle to remove tissue when an area is seen only on a mammogram.
- A small amount of local anesthetic (freezing) is injected into your breast with a needle. You will feel a sting.
- You will lie face down on a table and place your breast through a hole in the table. The breast is compressed in a mammography machine. You will feel some pressure in the breast.
- A small cut will be made in the area of the breast where the biopsy needle will be inserted. A sample of tissue will be taken (biopsy).
- A bandage is placed over the skin opening.
Other follow-up that may also be needed can include:
- surgical consultation, or
- magnetic resonance imaging (MRI).
3- Results
After your follow-up test(s), you will be notified by mail if/when you can return to BreastCheck for a screening mammogram. Most clients will have a normal follow-up test result and return to BreastCheck for routine screening. For more information about follow-up tests you can contact:
CancerCare Manitoba, BreastCheck
1-855-952-4325
Breast & Gyne Cancer Centre of Hope
1-866-561-1026
If you have these symptoms...
Know what looks and feels normal for your breasts. See your health care provider if you notice any of these signs or symptoms:
- puckering of the breast tissue
- a change in the nipple
- new or bloody discharge
- change in the size, shape or colour of the breast tissue
- thickened hard skin that feels different than the rest of your breast tissue, or
- a new lump
BreastCheck Mammogram Clinics
We mail you a letter to make a screening mammogram appointment every 2 years starting at age 50. A doctor's referral is not needed. Call 1-855-952-4325 to make an appointment.
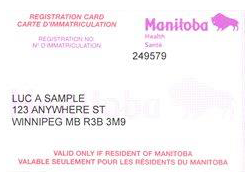
Bring your Manitoba Health Card to all your CancerCare Manitoba Screening appointments. Keep the information on your Manitoba Health card current. This will enable us to send you letters to remind you to get screened for cancer. To learn more, visit the Manitoba Health Card website.
BreastCheck has six clinics that accept appointments year-round. Two BreastCheck clinics are mobile and travel to nearly 90 rural and northern communities on a rotating basis.

BreastCheck Brandon
Old Nurse's Residence
620 Frederick Street
Monday - Friday
8:00 a.m. - 3:30 p.m.

BreastCheck Morden/Winkler
Boundary Trails Health Centre
Jct. Hwy 3 & 14, Winkler
Tuesday and Friday
8:15 a.m. - 3:15 p.m.

BreastCheck Thompson
Thompson General Hospital
871 Thompson Drive
Thursdays
8:30 a.m. - 2:20 p.m.

BreastCheck Winnipeg
Misericordia Parkade Building
#5-25 Sherbrook Street
Monday - Friday 8 a.m. - 5 p.m.
Saturday 8:00 a.m. - 3:30 p.m.
Upcoming BreastCheck Mobile Clinics
This tab is updated regularly with upcoming BreastCheck Mobile Clinic information. Site information is released up to 6 weeks in advance. For more information about an upcoming or future site, contact us at 1-855-952-4325 or email [email protected]
To share the posts below, follow us on Facebook, Instagram, and Twitter/X!
Killarney
Bayside Personal Care Home
86 Ellis Drive
December 2-5, 2024
Killarney BreastCheck Clinic Poster (pdf)
Beausejour
HEW Primary Health Care Centre
31 - 1st Street S.
December 2-20, 2024
Beausejour BreastCheck Clinic Poster (pdf)
Teulon
Teulon Memorial Hospital
162-3rd Avenue S.E.
December 30, 2024 - January 3, 2025
Teulon BreastCheck Clinic Poster (pdf)
Niverville
Niverville Heritage Centre
100 C Heritage Trail
January 7-9, 2025
Find A Mammogram Clinic
All clinics are wheelchair accessible. Make BreastCheck aware of any physical limitations when booking your appointment.
To find a mammogram clinic nearest to you:
- Enter your postal code or town/city name in the space below.
- Click on the magnifying icon to search.
GREY icons = not currently accepting appointments
PINK icons = currently accepting appointments.
BreastCheck Access Support
Group Trips
Communities can coordinate a group of people to attend a BreastCheck clinic at the same time for a series of consecutive appointments. Transportation to and from the BreastCheck clinic must be coordinated by the community/organization. For more information or to schedule a series of consecutive appointments (a.k.a. a group trip), contact BreastCheck at [email protected]
Transportation Support
Northern Patient Transportation Program
The Northern Patient Transportation Program (NPTP) subsidizes medical transportation costs for eligible Manitoba residents in the north to obtain medical or hospital care not available in their home community. Subsidies may include costs for an essential escort if required for a minor or a person with disabilities.
First Nations Transportation to BreastCheck through the Non-Insured Health Benefits Program
The Non-Insured Health Benefits Program offers coverage for travel to BreastCheck sites for registered First Nations clients.
Section 1.3 Medical transportation benefits may be provided for clients to access the following types of medically necessary health services
- publicly funded preventative screening such as breast cancer screening where coordination with other medical travel is not feasible
Clients, with the help of their health centres/nursing stations, are responsible for coordinating their travel through the Non-Insured Health Benefits Program.
Contact
1-855-95-CHECK (1-855-952-4325)
Interpreter services available upon request.
[email protected]
If you would like to promote any of our campaign videos, radio, and social media posts, email [email protected]