BreastCheck Information for Healthcare Providers
Most women age 50-74 should have a screening mammogram every 2 years. Trans men without chest surgery and trans women who have been on gender-affirming hormone therapy for a minimum of 5 years should also be screened for breast cancer.
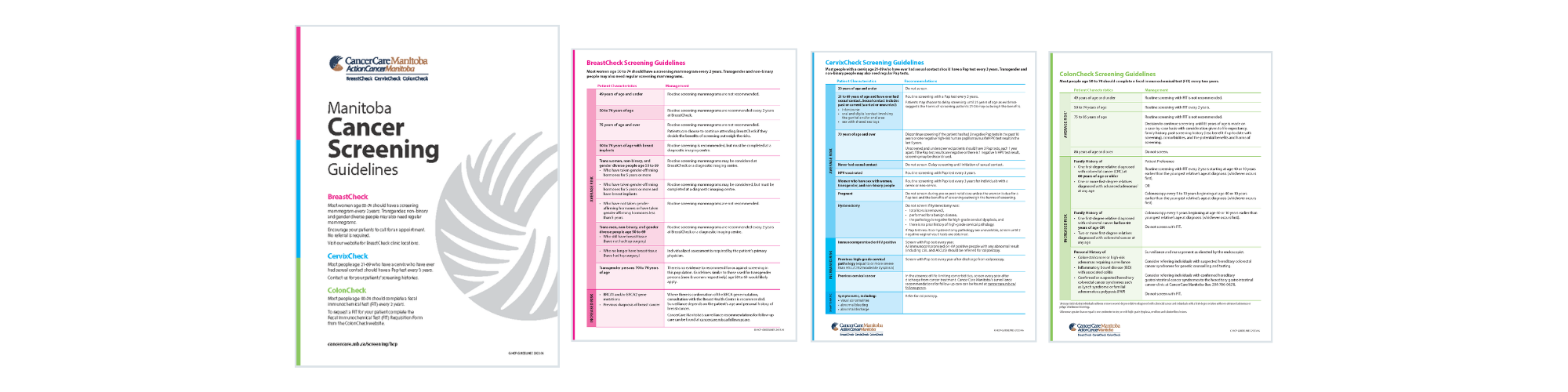
See the BreastCheck Screening Guidelines (pdf) for more detail.
Provider Resources
BreastCheck Screening Guidelines (pdf)
BreastCheck Results: Patient Discussion Guide (pdf)
BreastCheck Results: Patient Discussion Guide References (pdf)
Breast Health Services (pdf)
Recall Guidelines (pdf)
FAQ (pdf)
Clinic Resources
Breast cancer screening saves lives poster English | French
Honour your body, Know your breasts poster English
To download a poster for an upcoming BreastCheck Mobile clinic click here.
Patient Resources
Any resource with a star (*) beside it can be ordered from our online order form.
What you need to know about reducing your risk of dying from breast cancer (2021.06)
BreastCheck mammogram (illustrated version of the booklet above)
Breast Health: What is normal? booklet
Breast health services information sheet (11x8.5), (padded in 25s)
Compression information sheet
Radiation information sheet
Know your breasts bookmark
Forms
BreastCheck Appointment Form (pdf) - Last revised July 2020
Mammogram images are read by a radiologist the same or next day. Results are either normal or abnormal. In addition to the breast cancer screening result, the radiologist will also report the breast density category.
Normal
No abnormalities were found in the mammogram images. Approximately, 94% of BreastCheck results are normal.
BreastCheck will:
- Review the digital images and create a report with the findings.
- Send the breast cancer screening result (mammogram result and breast density category) letter to the client and healthcare provider within 2 weeks. The recommended interval for the next screening mammogram (one or two years) will be indicated.
Abnormal
Approximately, 6% of BreastCheck results are abnormal meaning that the mammogram image(s) showed something that the radiologist wants to examine further with follow-up test(s).
BreastCheck will:
- Review the digital images and create a report with the findings.
- Phone the client to notify them of their breast cancer screening result, and advise them of their follow-up diagnostic appointment within 5 days.
- Send the breast cancer screening result (mammogram result and breast density category) letter to the client and to their healthcare provider including information on their follow-up appointment.
- Follow-up tests
Breast Density Category
- Breast density is how breast tissue appears on a mammogram image. Breast tissue is made up of two types of tissue: glandular and connective (dense) tissue and fatty (non-dense) tissue. A person’s breast tissue may be called dense if they have more glandular tissue than fatty tissue. Breast density is measured by a radiologist using the Breast Imaging Reporting and Data System (BI-RADS). Breast density categories are grouped into one of four categories (a, b, c and d).
- To learn more about breast density, see the BreastCheck Results: Patient Discussion Guide (pdf).
Tell patients
- You will be provided information about the test, the appointment time, and directions to access the follow-up test(s) for which you are recommended.
- Maintain any follow-up appointments. Screening works best when you receive regular screening to monitor for any changes and attend all recommended follow-up testing appointments.
- If you require support during this time, you can contact the Breast and Gyne Cancer Centre of Hope at 204-787-2970 or toll free at 1-866-561-1026.
Resources to support result delivery and management
- BreastCheck Screening Guidelines (pdf)
- BreastCheck for Healthcare Providers: Results and Follow-Up (pdf)
- BreastCheck Results: Patient Discussion Guide (pdf)
Routine breast/chest cancer screening is every 2 years for most people.
Trans women, non-binary, and gender diverse people age 50-69:
- who have taken gender-affirming hormones for 5 or more years.
Recommendation: Routine screening mammograms at a BreastCheck site (no doctor's referral required) or a diagnostic imaging site (doctor's referral required).
- who have taken gender-affirming hormones for 5 or more years and have breast implants.
Recommendation: Routine screening mammograms at a diagnostic imaging site (doctor's referral required).
- who have not taken gender-affirming hormones or have taken gender-affirming hormones for less than 5 years.
Recommendation: Routine screening mammograms are not recommended.
Trans men, non-binary, and gender diverse people age 50-69:
- who still have breast tissue (have not had top surgery).
Recommendation: Routine screening mammograms at a BreastCheck site (no referral needed) or a diagnostic imaging site (doctor's referral required).
- who no longer have breast tissue (have had top surgery).
Recommendation: Individualized assessment is required at a diagnostic imaging centre (doctor's referral required).
Trans women, men, non-binary, and gender diverse people age 70-74:
- There is no evidence to recommend for or against screening in this population. Guidelines similar to those used for trans, non-binary, and gender diverse people age 50-69 would likely apply.
BreastCheck Access
- Those eligible for screening at a BreastCheck site can call BreastCheck at 1-855-95-CHECK (1-855-952-4325) to make a screening mammogram appointment.
To view the module in its entirety click here or click the individual chapter below:
Importance of organized breast cancer screening
Health promotion and education
Potential benefits and harms of breast cancer screening
Screening vs. diagnostic mammography

BreastCheck sends eligible people invitation, recall, and result letters based on the address information on their Manitoba Health Card. It’s important to remind patients to maintain their Manitoba Health Card information. If a patient moves they should update their Manitoba Health Card information with Manitoba Health at https://forms.gov.mb.ca/notice-of-change/index.html or by phone at 204-786-7101, toll free 1-800-392-1207, or through the deaf access line TTY/TDD at 204-774-8618.
No referral is required for an eligible patient to participate in breast cancer screening at BreastCheck. Patients should call BreastCheck at 1-855-95-CHECK to make an appointment. Patients call the same number to make an appointment regardless of the appointment location. Interpreter services are available upon request.
Click here to view all of our BreastCheck clinics including upcoming BreastCheck Mobile Clinic sites.
In determining an individual’s breast cancer risk, the following factors are considered:
- Age.
- Family history of breast and ovarian cancer.
- Personal history of lobular carcinoma in-situ (LCIS), atypical ductal hyperplasia (ADH), or atypical lobular hyperplasia (ALH), or breast cancer.
- History of radiation to the chest area in childhood or young adulthood.
To identify which patients at increased risk for breast cancer, see the BreastCheck Screening Guidelines (pdf).
Under age 50
Routine breast cancer screening mammograms are not recommended for people under age 50. People under age 50 who are at increased risk (personal or family history factors) or symptomatic should be referred to a diagnostic facility.
Under special circumstances, people under age 50 who are not able to reasonably access a diagnostic facility, may submit a request to be seen at a BreastCheck mobile clinic:
- The person’s healthcare provider must complete a BreastCheck Appointment Form and submit for review at least 4 weeks in advance of a BreastCheck mobile clinic.
- The BreastCheck Medical Lead will review and either approve or decline the appointment.
- BreastCheck will notify the requesting healthcare provider of the review result and required next steps.
History of breast cancer
Individuals with a family history of breast cancer can be seen at BreastCheck as long as they also meet BreastCheck’s eligibility criteria. At each mammogram appointment, the mammogram technologist will inquire about family history of breast and ovarian cancers. The answers provided will inform the frequency at which the client will need to be seen.
Individuals with a personal history of breast cancer require a referral by their healthcare provider to a diagnostic facility (not to BreastCheck) using the InSixty Breast Imaging Consultation Request form (pdf) and refer to a diagnostic site of your choice (see page 2 of the same form for a complete listing of diagnostic sites).
To view past and upcoming education and training opportunities, click here.
To be informed of upcoming education opportunities, we invite you to sign-up for our e-news.
CancerCare Manitoba Health Educators are trained professionals in a variety of disciplines including public health, education, and marketing. They provide education to the general public, underserved community groups, and training for community educators, and healthcare providers, about:
- Eligibility criteria for participating in breast, colorectal, or cervical cancer screening.
- How to access the various cancer screening tests.
- Potential benefits and harms of participating in cancer screening.
- Education, health promotion, and recruitment strategies for cancer screening.
Contact us at screening@cancercare.mb.ca if you have questions about cancer screening, resources, health promotion in your community, or education opportunities.
Contact
BreastCheck, CancerCare Manitoba
P: 1-855-95-CHECK (1-855-952-4325)
F: 204-788-1594
Stay Informed
We only send out e-news when we have something to share. Content includes changes to screening guidelines, new technologies, and education events.